The baseline examination in UK Biobank resulted in the collection of 68,151 paired colour retinal photographs and optical coherence tomography (OCT) scans from people aged 40 and 69. The number of people with eye data is being added to each year. UKBB therefore offers power to identify and quantify relationships between risk factors and eye disease in a community cohort of adults that is unparalleled worldwide. We aim to use the retinal photographs and OCT images collected from UKBB participants to study three of the most common eye diseases in later life- age-related macular degeneration (AMD), diabetic retinopathy (DR) and glaucoma. Supplementary studies of optic disc anomalies (congenital and acquired) and visual impairment associated with optic nerve and retinal anomalies are also underway.
Age-Related Macular Degeneration
Age-related vision loss is the major cause of acquired blindness in the western world. It affects over 30% of people over the age of 80 in Europe and the USA. In wet AMD (also known as exudative or neovascular AMD), treatment starts when some tissue has already been irreparably damaged. In atrophic, “dry” AMD, there is currently no approved treatment, although several clinical trials are being conducted. Therefore, prevention is the priority for for AMD management currently. However, effective prevention requires that modifiable, early-stage determinants of eventual visual loss be identified. A key early event leading to AMD is the appearance of sub-retinal pigment epithelial deposits (most often referred to as "drusen"), usually accompanied by pigment deposits in the retina. These changes are visible on retinal photographs.
Diabetic Retinopathy
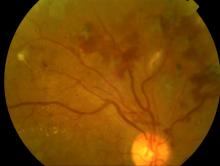
Diabetes is a common, life-long condition. There are 2.9 million people diagnosed with the condition in the UK. Blood vessels are especially sensitive to disturbances in blood glucose concentration. In the eye, this results in diabetic retinopathy (DR) - causing leakage of blood vessels, haemorrhages, lack of oxygen delivery (ischaemia) and scarring causing retinal detachments. Diabetes is the commonest cause of blindness in people of working age in the UK, and worldwide.
Aim of the study
To classify all retinal photographs in the UKBB dataset as normal, showing signs of disease or being ungradable.
To assess the frequency and characteristics of DR in known diabetics
To assess the frequency and describe the characteristics of AMD
To measure the cup to disc ratio - a widely-used marker of the presence or absence of glaucoma
To record the presence of any congenital or acquired abnormalities of retina or optic nerve
To explore how AMD, DR and glaucoma characteristics are associated with socio-economic factors, lifestyle and environmental exposures of participants.
To build a strategic resource for UK eye and vision research, and lay the foundations for long-term studies.
Retinal Image Grading
Retinal images will be graded by NetwORC UK. This scientific collaboration was established in 2004 by the UK's three main ophthalmic image reading centres (RCs): Moorfields Eye Hospital, London, Queen’s University, Belfast and Liverpool University. The network has a proven track record for analysing large sets. It has provided image grading for many large clinical trials and epidemiological studies. NetwORC UK’s administrative base (CARF, in Belfast) is responsible for the coordination of the RCs, leading management of datasets, training and generation of protocols. The 3 RCs share a unique common imaging and data entry platform, ensuring uniformity of output. In addition, joint teaching and training exercises for staff in the RCs and rigorous quality control ensures consistency of grading, reproducibility and reliability of image analysis.
